Vasectomy Reversal
Vasectomy is a highly effective form of birth control, and hundreds of thousands of men in the United States undergo this simple, safe procedure every year. Most men consider vasectomy a permanent birth control solution.
But if a man decides for whatever reason he would like to regain his ability to father children, there is a procedure to reverse vasectomy with the goal of regaining fertility.

Vasectomy reversals are routine nowadays, and although success isn’t guaranteed, many men go on to father children.
So what should men know about vasectomy reversal? This article covers what happens during this procedure, what recovery is like, and what men might expect as they go forward.
Anatomy review
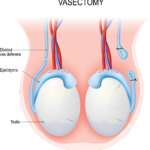
Both vasectomy and vasectomy reversal involve the route sperm cells travel from the time they’re produced to the time they’re mixed with semen. This pathway includes the following stops:
- Testes (testicles). Men have two testes, found together in a pouch called the scrotum. (The singular form of testes is testis.) The testes produce sperm cells and sex hormones, such as testosterone.
- Epididymides. Coiled on top of each testis is a long tube called the epididymis (this is the singular form of the word). After sperm cells are produced by a testis, they go to an epididymis to mature. They’re also stored there.
- Vasa deferentia. There are two vasa deferentia (the singular term is vas deferens or vas). Each vas connects an epididymis to the urethra. When a man becomes sexually aroused, sperm cells move from the epididymides through the vasa deferentia so they can be mixed with semen and be ejaculated out of the penis.
Vasectomy reversals are routine nowadays. Many men go on to father children.
During a vasectomy, each vas deferens is cut, blocking the sperm cells’ pathway and preventing them from mixing with semen. The sperm cells are not ejaculated; instead, they are absorbed by the body.
Vasectomy reversal undoes this process. During this procedure, each vas deferens is reconnected, once more allowing sperm to mix with semen and be ejaculated.

Preparing for a vasectomy reversal
Vasectomy reversals are usually done on an outpatient basis.
Vasectomy reversals are usually done on an outpatient basis. In the weeks beforehand, urologists give patients specific instructions on how to prepare, including whether certain foods or medicines need to be stopped before surgery. Some urologists recommend bringing tight underwear, compression shorts (i.e., stretchy, formfitting shorts most commonly used for exercise and made out of spandex, nylon, or polyester), or an athletic supporter for greater comfort afterward.
Men usually go home the same day, but because anesthesia is given, it’s essential to have a family member or friend do the driving. The procedure generally takes two to four hours.
Two types of vasectomy reversal procedures
The vasa deferentia are tiny tubes, and the stitches used in surgery can be thinner than an eyelash. For these reasons, most urologists use a special microscope during vasectomy reversals. This microscope can magnify the surgical area up to 40 times its original size.
Once anesthesia (general or local, depending on the situation) has taken effect, the procedure can begin.
Vasectomy reversals usually start the same way, with a small incision in the scrotum. Through this incision, the surgeon can access the ends of the vasa deferentia, which were cut during the vasectomy.
The surgeon gently pulls one pair of cut ends through the incision. Next, they check to see if there are sperm cells in the vasal fluid in the section of vas that is closest to the testis. The presence or absence of sperm cells will determine the surgeon’s next steps.
If sperm cells are present:
The two ends of the vas can be reconnected. This procedure is called a vasovasostomy. The ends of the vas are trimmed of any scar tissue from the previous vasectomy. Then, the surgeon sews them together. Afterward, sperm cells can flow through each vas like they did before the vasectomy.
If sperm cells are not present:
This means there could be a blockage from scar tissue between the testis and the end of the vas. In this case, a vasoepididymostomy is done. The surgeon makes a small incision in one of the coils of the epididymis. The other end of the vas is sewn so that sperm cells can travel straight from the epididymis to the vas, bypassing the blocked section of the vas. The longer it has been since vasectomy, the greater the chances that man will need this type of surgery.
Once one vas is reconnected, the surgeon works on the other one, following the same procedure. Sometimes, there is a block in one vas and not the other. When this happens, a man might have a vasoepididymostomy on one side and a vasovasostomy on the other.
After surgery, incisions are closed with stitches, and the area is bandaged.
Recovery after a vasectomy reversal
For most men, recovering after a vasectomy reversal isn’t a big deal. Any pain can usually be managed with over-the-counter medications, and applying an ice pack to the area can reduce swelling.
After resting at home for a few days, most men are back to their typical routine within a week. However, it’s still important to follow the doctor’s specific instructions.
Urologists usually recommend the following:
- Wearing tight-fitting underwear or an athletic supporter to hold the scrotum in place as it heals. Men may need to continue this support for a few weeks.
- Keeping the surgical area as clean and dry as possible. It’s best not to get the surgical site wet for two days. Doctors will advise on how to clean the area and when it’s okay to shower, bathe, and swim.
- Sports and other activities that could jostle or put strain on the scrotum (including heavy lifting) should be avoided for six to eight weeks.
- Men who work desk jobs can usually return to the office within a few days. The wait may be a little longer for men who work physically demanding jobs and those who do a lot of walking or driving.
- Sexual activity, including intercourse and masturbation, should be avoided for two to three weeks.
Vasectomy reversal complications
Complications from a vasectomy reversal are rare. But all medical procedures do carry some degree of risk. Some possible complications are:
- Chronic pain
- Bleeding in the scrotum
- Infection
About 5% of men develop scarring in the reconnected section of the vas. This scarring can block the sperm cells pathway again. In these cases, a second reversal procedure might be needed.
Men who experience any of these complications should call their doctor.

Getting pregnant after a vasectomy reversal
Once a man has a vasectomy reversal, is pregnancy a sure thing?
It depends. There are several factors to consider:
- Type of reversal procedure. Men who have a vasovasostomy may have sperm in their semen within three months. But for men who have a vasoepididymostomy, it’s usually a longer wait—up to 15 months, for some men.
- Time between vasectomy and reversal. The time frame between the original vasectomy procedure and the reversal procedure is important, as the chances of finding sperm in the semen decrease with time.
For example, one study has shown that 97% of the participants who had their reversal procedure less than three years after their vasectomy had sperm in their semen.
In contrast, 71% of the participants who had their reversal procedure 15 years or more after their vasectomy had sperm in their semen.
- Health of sperm. Sperm motility (the ability to swim to an egg cell) and morphology (its shape and the size of its head) are important factors. Good swimmers that are well-formed are more likely to fertilize egg cells. Men are encouraged to see their urologist for a semen analysis about six to eight weeks after a vasectomy reversal. This test can give more information about sperm health.
- Man’s overall health. A man’s health and lifestyle influence the quantity and quality of the sperm he produces. Certain illnesses (like diabetes, cancer, and multiple sclerosis) and medications (such as drugs for high blood pressure and depression) can affect sperm production. So can lifestyle habits, like smoking, drinking alcohol, and using recreational drugs. (Learn more about male infertility.)
- Partner’s age and overall health. When women reach their late thirties, they are less likely to become pregnant, as egg cells become less viable with age. Health problems—such as uterine fibroids, endometriosis, and diabetes—can also affect a woman’s fertility. But that doesn’t mean older women can’t have healthy pregnancies. Women are encouraged to see their doctor to discuss their fertility situation.
Resources
Cleveland Clinic
“Vasectomy Reversal”
(Last reviewed: June 6, 2022)
https://my.clevelandclinic.org/health/treatments/15459-vasectomy-reversal
“Vasectomy Reversal: Facts You Need To Know”
(September 13, 2022)
https://health.clevelandclinic.org/how-reversible-are-vasectomies/
“What’s the Best Age To Get Pregnant?”
(January 21, 2022)
https://health.clevelandclinic.org/best-age-to-get-pregnant/
Harvard Health Publishing
“Vasectomy”
(April 1, 2019)
https://www.health.harvard.edu/medical-tests-and-procedures/vasectomy-a-to-z
Healthline.com
Jewell, Tim
“Vasectomy Reversal: What You Need to Know”
(Updated on December 14, 2017)
https://www.healthline.com/health/vasectomy-reversal
The Journal of Urology
Belker, Arnold M., et al.
“Results of 1,469 Microsurgical Vasectomy Reversals by the Vasovasostomy Study Group”
(Abstract. Published: March 1, 1991)
https://www.auajournals.org/doi/10.1016/S0022-5347%2817%2938381-7
Mayo Clinic
“Female fertility: Why lifestyle choices count”
(May 5, 2022)
https://www.mayoclinic.org/healthy-lifestyle/getting-pregnant/in-depth/female-fertility/art-20045887
“Vasectomy reversal”
(August 20, 2021)
https://www.mayoclinic.org/tests-procedures/vasectomy-reversal/about/pac-20384537
Urology Care Foundation
“Vasectomy Reversal”
https://www.urologyhealth.org/urology-a-z/v/vasectomy-reversal
VeryWellHealth.com
Boskey, Elizabeth, PhD
“The Anatomy of the Epididymis”
(Updated: June 30, 2022)
https://www.verywellhealth.com/epididymis-anatomy-4774615